
Through collaboration with rural communities and practices, the iCARE project provides clinical services and practice support with a focus on innovative technologies. iCARE supports rural clinical practices through onsite primary care and subspecialty support, telemedicine, technical skills training, and community engagement.
Transportation barriers can be an impediment for rural residents with specialty care needs. This program provides boots-on-the-ground subspecialists, including pediatric subspecialists, maternal-fetal medicine specialists, psychiatry specialists, and adult cardiologists, to augment the care being provided in the local community. Clinicians also use telehealth or innovative models to expand local clinical services in rural communities.
iCARE Funding Opportunity
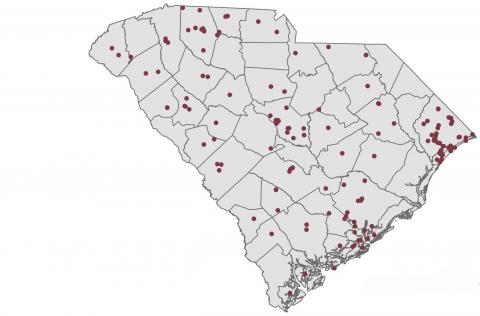
Map of Active iCARE projects
The Prisma Health Department of Pediatrics provides outreach clinics in rural communities in South Carolina. Subspecialty clinics include Cardiology, Endocrinology, Pulmonology, Nephrology, and more. Clinics are held throughout the midland's region including Aiken, Florence, Fort Mill, Lancaster, Orangeburg, and Sumter.
Increase the presence of pediatric Cardiology in Lancaster and Chester, SC as well as the surrounding rural catchment area with a rotating team of pediatric Cardiologists. Additionally, a team of forensic pediatrics provide services at Foothills Alliance Children’s Advocacy Center to help maintain access to service in Anderson, SC and the surrounding rural catchment area.
Provide adequate mental health care to underserved rural populations by providing psychiatric teleconsultations. Additionally, this program provides more opportunities for medical students and residents to have exposure to the capabilities of telemedicine.
This project aims to improve patient access to behavioral health care by establishing a collaborative care model of integrated care within the Family Medicine Center.
This initiative seeks to improve maternal and infant health in Saluda, SC by expanding its services to provide comprehensive prenatal care, delivery of the newborn, and post-partum care.
By educating primary care residents to provide prenatal care, this program will help improve access to prenatal care in rural, low-income communities that experience an absence of obstetrical care.
To improve access, this program will establish a prenatal clinic at Edgefield Medical Clinic to provide prenatal care for Edgefield County residents, especially those who live in underserved communities and have trouble traveling for prenatal care.
This program targets and engages a range of key healthcare providers in rural areas to provide educational materials, training, and capacity-building services using the Extension for Community Healthcare Outcomes (ECHO) model.
The Antimicrobial Stewardship Collaborative of South Carolina is a statewide partnership aimed at improving antimicrobial stewardship. Led by the University of South Carolina School of Medicine, Prisma Health-Midlands, the University of South Carolina College of Pharmacy, and the South Carolina Department of Health and Environmental Control, it unites healthcare providers across South Carolina.
This initiative supports a laborist model of obstetric care in which there is continuous, 24-hour coverage of the labor and delivery unit at a rural hospital.
In an effort to extend primary care services throughout the local community of Bamberg, SC, this program allows one full-time provider to focus solely on providing services through telehealth.
This clinic program tackles issues such as limited access to medical care, lack of health insurance, and transportation difficulties by offering free medical services. It includes expanded adolescent and mental health services and serves a significant percentage of American Indians.
This program focuses on the small/rural/underserved community healthcare providers who often struggle to find technology staff to manage their IT environments/infrastructure that is required in today’s world to help them manage the clinical needs of their patients.
This program aims to target the well-being of the staff tasked with the critical role of providing mental health services.
This initiative expands access to specialized care for COPD in rural areas with a provider specialized in respiratory disease management.
This initiative integrates a rural pharmacy residency program within Hope Health, combining clinical education and training with direct patient care. Its goal is to build the necessary infrastructure and capacity to launch a community-based postgraduate residency program.
This program uses telehealth to improve access to genetic care for children up to three years old with developmental delays across South Carolina.
This pilot project will develop and implement a maternal health training program and toolkit to increase pharmacists', student pharmacists', and technicians' capacity to improve maternal health outcomes in rural communities across South Carolina.
Promote early Hepatitis C intervention and treatment through case consultations and FibroScan referrals. Provide expert infectious disease collaborative care with the Southeast Viral Hepatitis Interactive Case Conference for patients in underserved rural areas of South Carolina and neighboring region. Additionally, the program will give providers access to evidence-based education to optimize the health outcomes of patients.
Embeds a Community Health Worker within the local care teams at two medical clinics in Chester, SC to improve community resource utilization and chronic disease outcomes. CHW will integrate health care and community programs by providing patients of each clinics with tailored recommendations and conducting referral follow-ups.
Provides support for Family Medicine practices in Winnsboro and Bishopville to ensure those vital services are available in those communities.
Provided acute neurological care to approximately 400 patients per year in Sumter, SC, and reduced the number of neurology service-related transfers.
Implemented primary care providers in under-resourced, rural counties with a high incidence of HIV into a PrEP clinic that offers technical support with on-site visits, provides a tailored PrEP provider toolkit, and invites participation in PrEP Teleconsultation.
This program seeks to onboard a pharmacist at Fairfield Medical Associates, a designated rural health clinic, to replicate the patient-centered outcomes and financial sustainability of the evidence-based clinical pharmacist model implemented by a small rural health clinic in Bamberg, SC.
This project utilized mobile health units to provide care to rural and uninsured individuals with opioid use disorder (OUD) and/or hepatitis C (HCV) in the Upstate and Midland regions of South Carolina.
This project established a prenatal care clinic at its rural residency site in Cheraw, SC. Residents received hands-on training on providing prenatal care in a rural community while providing access to services in an area with significantly fewer options for prenatal care than their urban counterparts.
